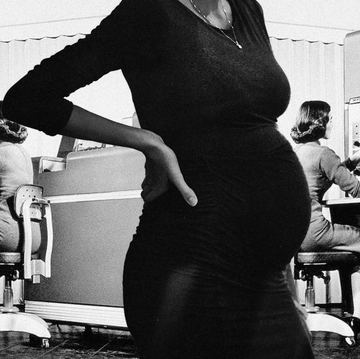
A year ago, my brain was locked on autopilot: I have to lose weight to have a baby, which will make me gain weight. I have to lose weight to have a baby, which will make me gain weight. I have to lose weight to have a baby, which will make me gain weight.
The thought kept looping in my head, over the droning of my sixth IVF consult—over Zoom, no less—in a two-year span. Today, the doctor says my vitals and blood work are perfect but my weight less than (well, really, more than). For that reason alone, she will not treat me. This meeting is not going well. And I can’t overstate how much a pandemic complicates trying to conceive when your eggs are aging like week-old milk. I was navigating telehealth appointments, fighting my insurance company over billing, and chasing overworked doctors for just a little bit of clarity.
Remember how in Kill Bill, every time Uma Thurman as Beatrix Kiddo meets her opponent, she sees red? Her eyes narrow, and her brow furrows as she lasers in, thunderous funky synth wailing in the background?
When the doctor says from the other side of the screen, “Again, Wynter, everything looks great. It’s just your BMI. We gotta get some weight off,” I am Beatrix, seeing red. Excuse me, who is “we”? Not another tense, emotional midday conversation with the onus back on me to wrestle with a body that already feels like it isn’t cooperating. It doesn’t matter to this doctor that BMI is a hugely flawed metric of health or that the research on the relationship between weight and successful embryo retrieval is mixed—many fertility specialists have a firm BMI cutoff, after which they will not treat patients.
After enduring three medically necessary abortions of very wanted babies in just 18 months, having the word “weight” thrown around—and so coldly—pushed me over the edge. I was done. I launched into a sobbing rant, laden with many F-words and zero regrets. I wanted to dramatically slam down the phone. Instead, I cut her off mid-sentence and tapped the END MEETING FOR ALL button and fell silent.
Growing up, I always battled with both my body and body image. As a child of the ’80s, the ideal of beauty was waifish and white, like Christie Brinkley and Brooke Shields—they didn’t look like me. As a curvy teenager, I obsessed about my body daily, if not hourly. From fad diets to abject shame, I tried to punish it into submission. At 17, I received a diagnosis of polycystic ovarian syndrome well before it was understood (even in the medical community), which explained why I struggled with my weight. Still, there was no easy treatment or solution.
In my mid-20s, I worked hard to unlearn all the toxic noise around thinness and beauty standards, and by the time I was in my 40s, I had arrived at some semblance of peace. The reality is having curves never stopped my hustle. I knew I could be beautiful, sexy, and successful all the same (and my husband, Allan, agrees). But trying to get pregnant challenged all of those hard-won gains. My own fraught path to starting a family eventually led me to Ozempic, one in a class of new, cutting-edge drugs with weight-loss benefits that have exploded in popularity in the last year. The rise of these drugs has ignited a fierce and messy debate about health, bodies, and fatphobia (not to mention sending the Hollywood gossip machine into hyper-drive).
I can only speak to my experience, but taking Ozempic allowed me to reset my relationship with my body and focus on taking care of it. The cultural furor around these drugs—Are they good? Are they bad? Should everyone take them? Should no one take them?—flattens all those nuances and does a disservice to those of us who are trying to make a compassionate decision for ourselves among a lot of less-than-ideal options. That IVF doctor had never seen me in person, hadn’t examined me, or done more than glance at my records, but in her mind, my weight was the only thing holding me back from a successful pregnancy. I’m confident that wasn’t the right answer or manner of delivery, but that was the reality I was facing.
After that last appointment, knowing that weight loss would fast-track my egg retrieval sent me into a downward spiral that felt all too familiar. From behind my desk, I looked in the mirror and thought, You are failing me—AGAIN. It didn’t matter that the weight I had gained recently was partially from my lost pregnancies. I turned all my disdain on myself. To add another layer to all of it, I didn’t love the habits I had formed during the pandemic: everything from working exclusively from my couch to relying far too much on takeout and making viral recipes. I became a recluse, finding excuses not to see my friends and family, all the while obsessing about my body’s perceived failures.
Resenting the prognosis but committed to a solution, I gave myself three months to focus on my health so I could get into a facility quickly to retrieve. Yes, I wanted to get to this “golden BMI” but more than that, I didn’t want my weight to always be at the front of my mind, a constant hang-up that kept me from the happiness I knew I deserved.
This time, I was over 40 and out of ideas. My inner dialogue was as feisty as ever, laying it all on the line, aggressively persuasive. I thought about the diet pills I had tried when I was 16, which had given me waking dreams. I remember how taking up smoking in my 20s kept my mind off of food and knew I couldn’t (and wouldn’t) go back to that. Then there were all the “L.A. trends”: liquid diets, intermittent fasting, B-12 shots, and so on.
All of that thinking was unhealthy and unhelpful. Frustrated, I turned to an online community I joined for women over 40 trying to get pregnant and shared that my BMI was considered too high to retrieve. Refreshing the page over and over, in between supportive comments like “Ew! New doctor, pls” and “I’m so sorry sweetie,” someone chimed in, “Ozempic?” Ozempic. The one from the commercial? Isn’t that to control diabetes?
Formally called semaglutide, Ozempic is indeed intended for sufferers of type 2 diabetes because it lowers blood sugar by mimicking a hormone that is typically released after eating. After clinical trials showed that it also had significant weight-loss benefits, the FDA has also approved a dosage of semaglutide (under the brand name Wegovy) for weight management. Depending on the prescription, patients typically receive a pen that allows them to self-inject weekly.
I was skeptical. I’d done the right (and wrong) things my entire life to try and lose weight, and it had continued to come back. But at this point, I was willing to try almost anything. Since I also suffer from insulin resistance, which mimics pre-diabetic symptoms, a doctor quickly approved my prescription, and it was covered by health insurance. It arrived in the mail a week later, packed neatly in a white box. Ripping it open, I administered it immediately. But the idea of failing at this—and at this point, it all felt like failure—made me emotional. Another pandemic side effect: crying on a dime. When I crawled into our bed, Allan held me close and told me, “I love you no matter what. Period.” Still, with the broken record in my brain, I obsessed over the expectation of the shot and braced myself again for disappointment.
Three days later, I realized I was eating less and not really “thinking” about it. That feeling of satiation, instead of planning the next meal mid-bite, allowed me to concentrate on other things. It was easier to make good choices and drink less wine. I was no longer punishing myself or using food to guide my moods. My sleep was better, and I felt more energized, although I did also experience waves of nausea, a common side effect of Ozempic. The weight began to come off. I was stoked. My mood made it easier to reintroduce my favorite exercise, weights, and cycling into my routine and to speak more kindly to my body.
For the first time in decades, there was a way to manage my PCOS, which is known to disrupt the body’s cues for hunger and fullness, that worked for me. One of the most remarkable things was how taking Ozempic highlighted how much I had been fighting my body—and belittling it—instead of caring for it. Within two months, I was over halfway toward my weight-loss goal. Success felt tangible for once.
Months after I started Ozempic, I paused the treatment. After searching for a new IVF doctor in Southern California who I hadn’t screamed at (it was not easy), I found one in Santa Barbara who was refreshingly anti-BMI and willing to treat me at any weight. Still, I’m glad I went on Ozempic. The reality is that when it was really time to start the grueling IVF process, I felt more mentally and physically prepared for it—no longer sluggish, achy, or depressed. Do I think it helped my embryo quality? Not really, but I do think it disconnected the cycle of shame and self-recrimination I was stuck in so that I could actually focus on my overall wellness.
After the usual exams and ovarian stimulation, Allan and I got five embryos. I didn’t freak out about the 10 pounds I gained from the procedure—I was just thrilled to enter the new year with these gifts and proud of what my body was able to accomplish.
But I want to be clear: I don’t want to be thin. All I want is a good life.
While it’s gotten a little better from when I was growing up, this culture sometimes makes this impossible—gaining weight is considered some sort of moral failure, especially for women. And wanting it off doesn’t mean we don’t love ourselves. It’s a double-edged sword that cuts deep. There’s also not enough awareness of all of the hurdles women over 40 must get past to have a baby.
But one size doesn’t fit all and this medication isn’t the final answer. Take Ozempic, don’t take Ozempic—it’s your lane and you have to cruise at a speed that works for you. It can all be disorienting—in this weird moment of cutting-edge medical innovation and peak cultural confusion with a big heap of double-talk and gossip, many don’t have the luxury or energy to fight for the care they deserve. My hope is that ultimately, we can move into a place where everyone’s health is taken seriously without judgment. Most importantly, I hope we can all be given the space to make decisions that are right for us.
Wynter Mitchell-Rohrbaugh is a digital strategist, writer, and podcast host/producer for Waiting To X-Hale and the upcoming Tangent Island. She has written and discussed pop culture, digital evolution and social impact in Cosmopolitan, Yahoo, BlogHer, THR, Cheddar The Independent, San Francisco Chronicle, NPR, WNYC and Variety. She hails from San Francisco and lives in Los Angeles, CA. Follow her on Twitter @wyntermitchell.